7667766266
enquiry@shankarias.in
Why in news?
A recent study published stated that the prevalence and morbidity of NCD in India has been increasing in the past decade.
What is non-communicable disease (NCD)?
|
Status of NCDs in India |
|
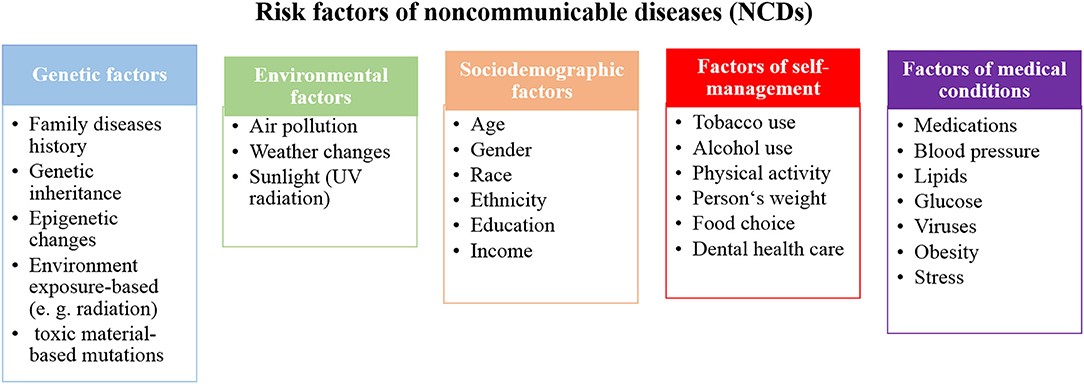
What are the Risk factors for NCDS?
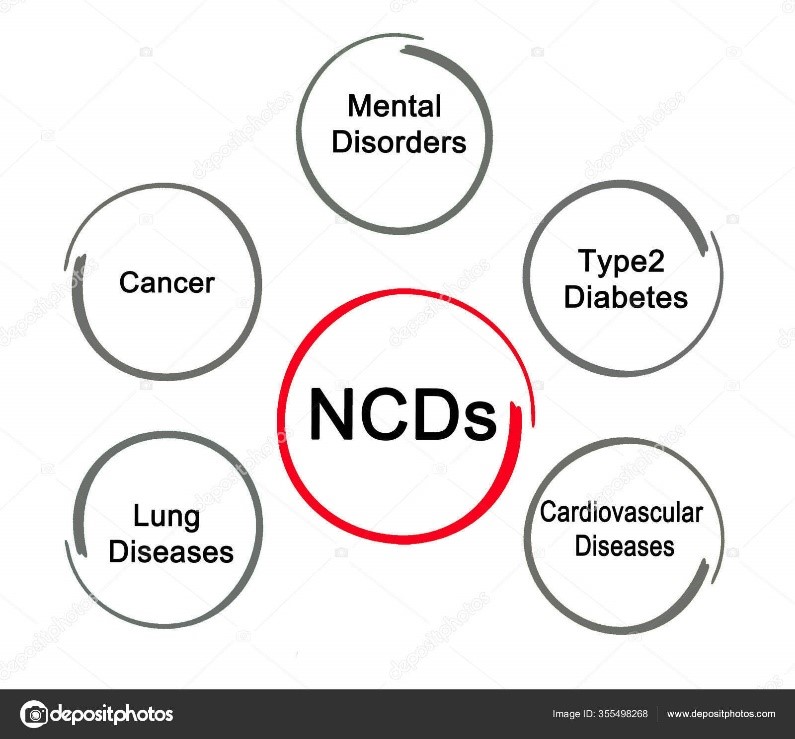
What are the types of non-communicable diseases?
What are the effects of NCDs?
|
Government Measures in India |
|
What are the measures to address NCD?
ASHAs are trained to work as an interface between the community and the public health system.
References