7667766266
enquiry@shankarias.in
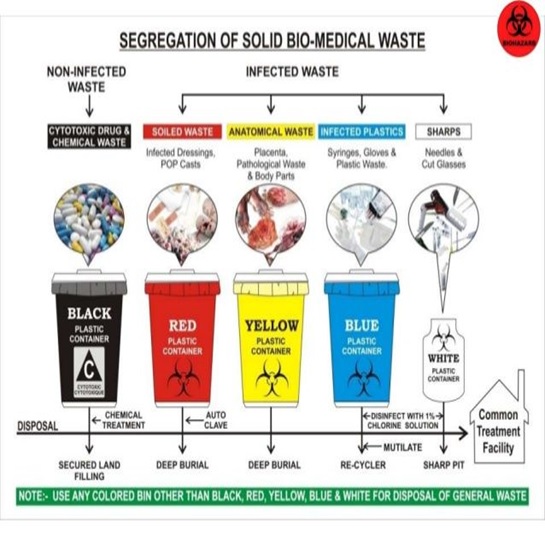
Growing medical waste is causing serious ecological consequences before and after the covid-19 pandemic.
|
Hazardous waste |
Non-hazardous waste |
|
|
|
Biomedical Waste Management Rules 2016 |
|